Revealing the Alarming Economic Burden of Tuberculosis Treatment in India
A recent study published in PLOS Global Public Health has unveiled the staggering financial burden that tuberculosis (TB) patients in India face. Conducted by researchers from The George Institute for Global Health India, in collaboration with Indira Gandhi Government Medical College (Nagpur) and the London School of Hygiene and Tropical Medicine (UK), the study paints a grim picture of the economic toll of TB on affected households.
Background: The Global TB Crisis
Tuberculosis remains one of the world’s deadliest infectious diseases. According to the World Health Organization (WHO), 10 million people fell ill with TB worldwide in 2020, with India accounting for the highest burden at 2.42 million cases in 2022. The WHO’s End TB strategy aims to reduce TB incidence, mortality, and catastrophic costs associated with the disease by 2035. However, as the recent study highlights, India is still grappling with significant economic challenges for TB-affected households.
Methodology of the Study
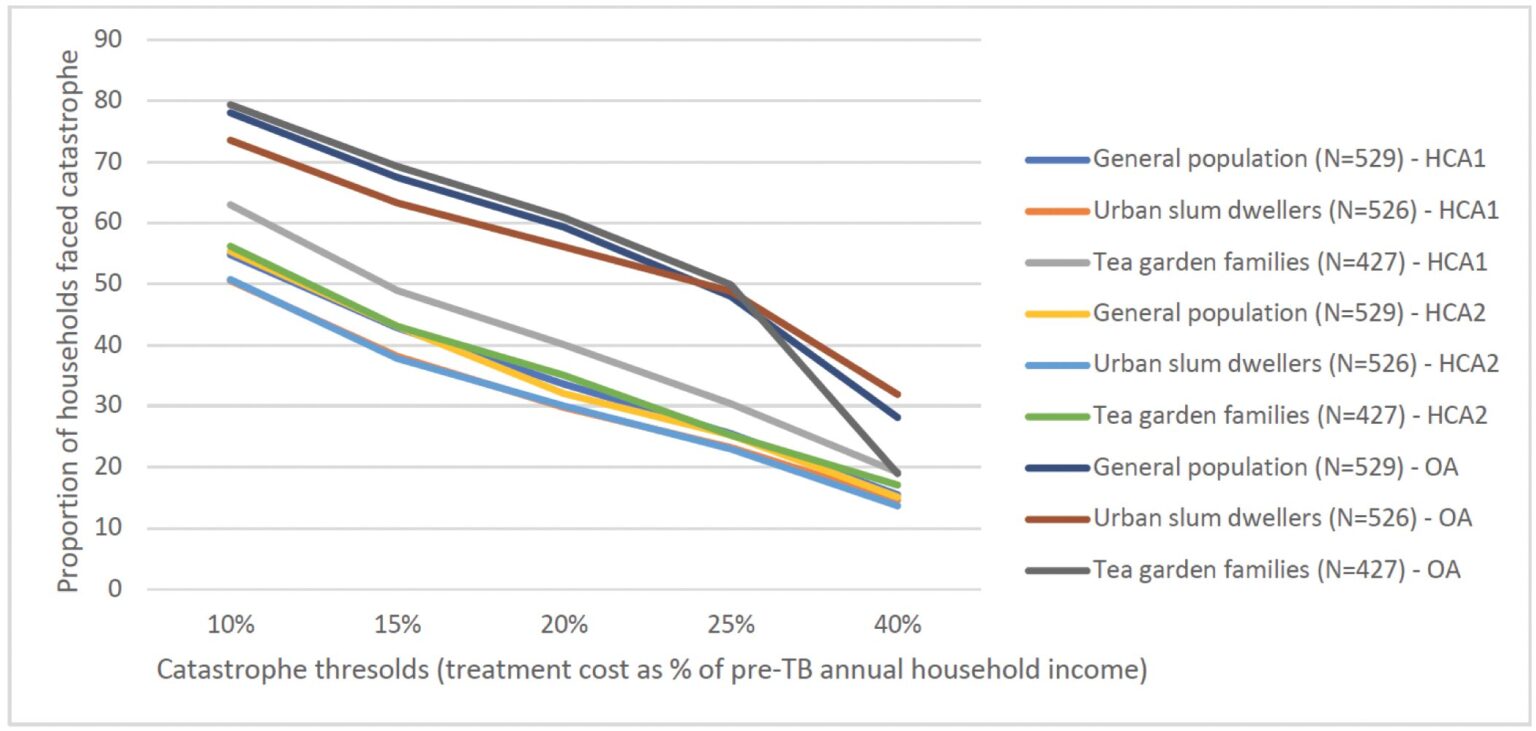
The researchers followed a cohort of 1,482 drug-susceptible TB patients across Assam, Maharashtra, Tamil Nadu, and West Bengal. Utilizing WHO guidelines, the team calculated both direct costs (actual money spent) and indirect costs (time, productivity, and income loss). The study explored three different methods for calculating indirect costs:
- Human Capital Approach 1 (HCA1): Valued hours spent using the minimum wage rate for all.
- Human Capital Approach 2 (HCA2): Valued hours spent using a combination of the patient’s wage and minimum wage.
- Output Approach (OA): Focused on lost productivity as output loss.
Key Findings
Dr. Susmita Chatterjee, the lead researcher from The George Institute for Global Health India, stated, "Our study concluded that a significant proportion of study participants faced catastrophic cost, and the proportion was much higher when income loss due to TB treatment was included." According to the study, depending on the indirect cost calculation method used, between 30% to 61% of participants faced catastrophic costs. These costs exceed 20% of a household’s pre-TB annual income, jeopardizing their financial stability.
Pre-Treatment Financial Burden
One of the most alarming revelations of the study is that over half of those who faced catastrophic costs encountered these expenses even before starting TB treatment. An average delay of 7-9 weeks from symptom onset to treatment initiation meant repeated consultations, diagnostic tests, and travel expenses, which exacerbated financial strain.
Policy Implications and Recommendations
The study’s findings call for urgent interventions at both policy and community levels:
- Private Sector Engagement and Rapid Diagnosis: Intensifying private sector involvement and streamlining diagnostic processes can help in early detection and treatment, mitigating pre-treatment costs.
- Community Awareness Campaigns: Informing communities about TB symptoms and the importance of early medical consultation could reduce diagnostic delays.
- Reimbursement of Pre-Treatment Expenses: Integrating TB-related expenses into health insurance plans can help alleviate the immediate financial strain on households.
- Employment Safeguards: Implementing policies to protect TB patients from unemployment and income loss during their treatment period is vital.
In light of these findings, concerted efforts from policymakers, healthcare providers, and communities are essential to alleviate the economic burden of TB treatment in India. These strategies not only aim to reduce financial hardships on patients but also align with the global goals of the WHO’s End TB strategy.
For more information, visit The George Institute for Global Health at www.georgeinstitute.org.in.
Source: Susmita Chatterjee et al., Catastrophic costs for tuberculosis patients in India: Impact of methodological choices, PLOS Global Public Health (2024). DOI: 10.1371/journal.pgph.0003078